Drug discovery
Work with us to identify and advance novel approaches with the potential to deliver the next generation of cancer medicines.
How scientific expertise, funding and entrepreneurship came together for the development of an antibody-drug conjugate targeting lymphoma.
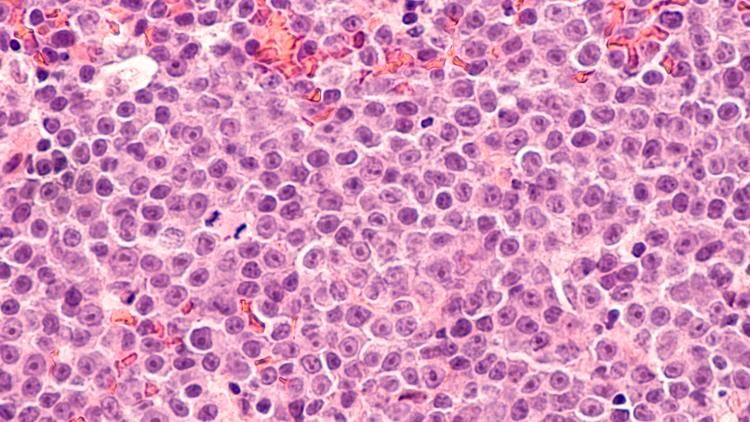
Oncologists treating diffuse large B-cell lymphoma (DLBCL) have a new medicine in their armoury. In April 2021, following impressive Phase 1 and 2 clinical trial data, the FDA gave accelerated approval to Zynlonta for treating patients with refractory or relapsed forms of DLBCL.
The drug, developed by Switzerland-based ADC Therapeutics (ADCT), will still be monitored in a final confirmatory trial but its entrance into the clinic marks an important milestone – not just for treating DLBCL, but in heralding too the arrival of a new type of therapy.
Zynlonta (loncastuximab tesirine-lpyl) is an antibody-drug conjugate, or ADC – a complex therapeutic agent in which an antibody carries a cytotoxic drug specifically to cancer cells. Once the ADC binds to those target cells, it’s internalised by them. Then, in the cells’ lysosomes, the cytotoxic drug component – commonly referred to as the warhead – is cleaved from the antibody. Liberated, the warhead diffuses to its site of action, disrupting a vital cellular function – blocking mitosis in the case of Zynlonta – and killing the malignant cell.
Paired with different antibodies, PBD warheads will hopefully lead to a host of new drugs for a range of haematological and solid tumours
Zynlonta is the 10th ADC to gain FDA approval – this therapeutic strategy having slowly, then rapidly, gained pace over the last 20 years. The drug targets the cell surface marker CD19, which is selectively expressed on B cells and is already a cornerstone of CAR T-cell approaches to treating B-cell lymphomas.
More significantly, Zynlonta is the first ADC to use a novel type of warhead comprised of a PBD (pyrrolobenzodiazepine) or, more specifically, a PBD dimer.
PBD dimers potently cross-link DNA and prevent cell division. The developers of Zynlonta believe it’ll be just the first in a succession of approved ADCs deploying this chemical innovation. Paired with different antibodies, PBD warheads will hopefully lead to a host of new ADCs for a range of haematological and solid tumours.
ADCs work through the coupling of two different elements, each vital. This story began, however, with a meeting between a chemist and a biologist, each of them just establishing their own labs.
In the early 1990s, biologist John Hartley was working at UCL investigating exactly how various DNA-targeting chemotherapy agents functioned. And medicinal chemist David Thurston was at the University of Portsmouth experimenting with PBDs. Both were funded by The Cancer Research Campaign – one of the two charities that merged to form Cancer Research UK in 2002.
This class of DNA-binding chemicals had been originally isolated from bacteria in the 1950s and had received a steady stream of attention from medicinal chemists because they uniquely bind to DNA’s minor groove – but without ever leading to a useful drug.
Thurston was interested in the possibility that conjoining two PBD units in just the right way might yield a dimer that could bind not one DNA strand, but two. Such a molecule, he reasoned, would cross-link DNA and very effectively suppress mitosis.
Early ADCs represented key proofs of concept, but it was clear that they could be improved on – the idea behind them may have a simple elegance but it demands a challenging pharmacology
These were the early days of using molecular modelling to design novel compounds, Thurston says, and this nascent computational approach seemed to pay off. But to prove that the new dimers he created functioned as he intended, Thurston needed a partner who was expert in DNA biology.
Hartley and Thurston met at a conference and immediately saw how they could complement each other’s work. After they published their first paper showing the new PBD dimers cross-linked DNA and were cytotoxic, CRC funded a pivotal collaboration between the pair.
“We didn’t know if you made PBDs twice as big and put linkers on them, if you’d lose all their DNA-binding properties. There was a lot of development work,” Hartley says. As he tested the molecules' biological effects, Thurston made new dimers. “We medicinal chemists call it decorating the molecule,” he says.
Their combined work showed that the compounds, indeed, cross-linked DNA effectively and selectively. Not only that, they did so somewhat stealthily, so as to not recruit the DNA repair mechanisms that often limit the effectiveness of other DNA targeting cancer drugs.
“Because the results got more and more interesting,” Thurston says, “this led to a five-year programme grant with Cancer Research Campaign.”
Soon, the collaborators moved to test the compounds’ efficacy in cancer models. At this point, the PBD dimers were envisaged purely as systemic agents that would kill cancer cells as traditional chemotherapeutic agents did – by exploiting rapidly dividing cells’ sensitivity to disrupting DNA.
With Cancer Research Campaign leading the way, the most promising PBD dimers were sent to the National Cancer Institute in the US to be tested in their cancer cell line and animal models. These drugs, Hartley says, were “found to be some of the most active agents that they’d ever put through the screen”.
Soon after, in the late 1990s, Thurston got a phone call from Cancer Research UK's commercial partnerships wing saying they thought this work looked to be ripe for commercialisation by spinning out a company. Thurston and Hartley – with Phil Howard, the chemist who was by then leading the work in Thurston’s lab – agreed to this proposal. And soon the group was introduced to a potential CEO – biomedical entrepreneur Chris Martin.
“I was searching for a next-generation cancer therapy,” Martin says, “and had seen many growth-inhibition curves – the PBDs produced flat lines in model after model.”
Immediately sold on the approach, Martin proposed a spin-out company with commercial rights to all the patents relating to this PBD dimer chemistry, that he, Hartley, Thurston and Howard would be co-founders of. The result was Spirogen – a London-based start-up founded in 2000 and still operating today, with Howard as Chief Scientific Officer.
Some of the most promising ideas might be seen as too risky, too blue-sky, for many pharmaceutical companies which is why we're committed to supporting spin-outs develop
Cancer Research Horizons supported that initial spin-out by being amongst the original shareholders. And it is this fostering of commercial partnerships that we know is key to the development of therapeutics. “We want to advance discoveries to beat cancer by developing and commercialising exciting new ideas,” says Tony Hickson, Cancer Research Horizons' chief business officer. “We have a real understanding of both academia and industry, so we are in a great position to translate promising research. We also know some of the most promising ideas might be seen as too risky, too blue-sky, for many pharmaceutical companies which is why we are committed in our support of the development of spin-outs.”
Securing the right relationship with Spirogen was very important for Hartley, who never wanted to jeopardise his academic career. His main challenge was in maintaining boundaries between his academic pursuits and Spirogen’s ambitions. But with a supportive head of department and Spirogen paying for dedicated staff in the lab, Hartley was soon happily running the business side of his lab alongside his Cancer Research UK-backed academic programme. “And it’s worked very, very well,” he says.
In the mid-2000s, Cancer Research Horizons and Spirogen began the first preclinical and early clinical testing of PBD dimers as standalone systemic agents, including the pharmokinetic studies through the Cancer Research UK-backed cancer research unit at the University of Bradford and a Cancer Research UK-sponsored Phase 1 clinical trial in the UK.
While the drugs showed some potential, low efficacy and problematic toxicities thwarted development as standalone agents. Hartley says in a way they’d been too clever, developing drugs so potent it was difficult to get clinical benefits without limiting side-effects. All of which prompted a major rethink.
With clinicians increasingly interested in targeted therapies, Spirogen soon settled on the idea of using their PBD dimers as warheads on ADCs.
The FDA first approved an ADC in 2000. This therapeutic class, in many ways, marked the realisation of a century-old ambition – formulated by Paul Ehrlich in the 1900s – to create a magic bullet for treating cancer: a means to deliver cell-killing chemicals specifically to malignant cells. “In theory,” Hartley says, “if you’ve got a completely tumour specific antigen, you should be able to deliver a drug only to the tumour cells and spare all normal tissue.”
Early ADCs represented key proofs of concept, but it was clear that they could be improved on – the idea behind them may have a simple elegance but it demands a challenging pharmacology. “There’s the antibody, the linker, and the drug. And you’ve got to get all three bits right,” says Hartley. “That’s why the field has been relatively slow to develop.”
We realised that PBD dimers were probably going to tick a lot of boxes for the warhead component of ADCs
For example, antibody and warhead must be attached in a way that diminishes neither of their activities. They need to remain tightly connected when outside of their target cells, but readily dissociate once inside. The antigen needs to be right, the antibody needs to be readily internalised and the whole ADC efficiently trafficked to the lysosome. And, of course, you require an effective warhead with chemistry to suit the application.
Hartley says, “We realised that PBD dimers were probably going to tick a lot of boxes for the warhead component of ADCs.”
US biotech Seattle Genetics had expressed an interest in using PBD dimer warheads and soon, Martin set up a partnership with them, followed by similar deals with Genentech and AstraZeneca.
However, in early clinical trials of PBD ADCs the shortcomings of the first warheads became clear.
Learning from the limitations of the first generation, Spirogen developed second and third-generation warheads – reducing their hydrophobicity and ultimately, investing mainly in the PBD dimer, tesirine. With newer warheads, the company changed tack – rather than licensing out a warhead for partners to use as they pleased, they licensed PBD dimers to partners to be attached to specific antibodies on a case-by-case basis.
But scientists in the company had, by then, developed their own expertise in linking PBD dimers to antibodies. “We now had two different things,” says Hartley. “We had the PBD dimer technology within Spirogen, and all the patents around that. But we also had the ability to make some ADCs ourselves.”
This led to two significant developments. In 2012 Martin led the spin-out of a second company: ADC Therapeutics, the developers of Zynlonta, of which he remains CEO.
Then, in 2013, Spirogen was acquired by MedImmune, a subsidiary of AstraZeneca, giving AstraZeneca control over the future development and licensing of PBD dimer warheads.
ADC Therapeutics had, however, been formed with the option of developing up to 11 PBD-containing ADCs. To choose which, Martin says, “we started with a blank sheet of paper and developed all of our pipeline therapies from the laboratory bench”.
They focused on both haematological and solid tumours. CD19 was chosen as a means of tackling DLBCL, and CD25 was selected for a second ADC – termed camidanlumab tesirine, or Cami – for Hodgkin lymphoma and solid tumours.
The first patient received Cami in October 2015, while the first dose of Zynlonta was administered in March 2016. Both proceeded smoothly through Phase 1 clinical trials and into Phase 2, albeit with Zynlonta’s more rapid success seeing it leapfrog Cami, in terms of approval.
In June 2020, ADC Therapeutics announced the results of their 145-person Phase 2 trial in refractory and relapsed DLBCL that won the drug its accelerated approval by the FDA. It showed that 48% of patients responded to Zynlonta, with 24% entering complete remission.
With Zynlonta approved and five ADC therapies in multiple clinical trials, many patients are benefiting from Cancer Research Horizons' investment which started over 20 years ago
In May 2021, they announced that 39 of 47 patients with relapsed and refractory Hodgkin lymphoma saw their cancers respond to Cami, with 18 of those, 38%, entering complete remission.
With these impressive results, the company anticipate Cami also being submitted for a biological licence application. “This has clinically validated the PBD dimer platform as a warhead,” Hartley says, “and hopefully it will lead to others, including in solid tumours.”
Martin certainly thinks it will – and he’s thankful for Cancer Research Horizons' vital early contributions. “With Zynlonta approved and five ADC therapies in multiple clinical trials in the UK, Europe and the US in haematological and solid tumours, many patients are benefiting from Cancer Research Horizons' investment which started over 20 years ago,” he says. “Cancer Research Horizons' initial investment has resulted in chemistry which has attracted over $1bn from capital markets, all of which has been invested in bringing new therapies to cancer patients.”
Hartley, as well as his essential contributions to the development of these drugs, has maintained a successful academic career throughout, finding many fruitful ways to pair his commercial work with basic research. Like Spirogen did, ADC Therapeutics has funded clinical fellows and PhD students in his lab, and – with their intellectual property legally protected – they’ve pushed those researchers to present at conferences and to publish. “I’m an academic,” Hartley says, “and I’m a great believer that when you can, the information needs to get out there. And that is Cancer Research Horizons' philosophy too.”
His group has published consistently on the pharmacology of both the PBD warheads and the more complex biology of the ADCs.
Pleasingly for him, things came full circle when some of the Zynlonta trials were conducted at UCL and his lab processed samples from patients. His lab was part of the Experimental Cancer Medicine Centre Network, jointly supported by Cancer Research UK, and using assays his lab had developed, they could directly measure DNA cross-links in target cancer cells. In fact, quantification of the warheads’ effects at the molecular level has become a central part of the development of PBD-containing ADCs, showing that they act exactly as they are designed to.
It’s taken a quarter of a century from the project’s conception to clinical approval, and he’s been involved throughout. “I wasn’t grey when I started, let’s put it that way,” Hartley jokes. For Cancer Research UK’s longstanding support – both to his PBD work and to his other projects – he’s very grateful.
“The most satisfying thing is that it’s going to benefit patients,” says Hartley, “If Cancer Research Horizons hadn’t been supportive, this day wouldn’t have happened. Their commitment to translational research has been shown.”
Professor John Hartley is Professor of Cancer Studies at the UCL Cancer Institute. He is a scientific advisor for ADC Therapeutics and scientific co-founder of Spirogen. He was also the Director of the Cancer Research UK Drug-DNA Interactions Research Group since 1995. For over 20 years he has been Chair of the Protocol Safety & Review Board (formerly the Central Institutional Review Board) which is the early clinical trial protocol review and ethics committee of Cancer Research UK. He is Co-Centre Lead of the UCL ECMC and Head of the UCL ECMC GCLP Facility, a CRUK Centre for Drug Development Biomarker Centre of Excellence. Professor Hartley is a Fellow of the Royal Societies of Biology and Chemistry, a Fellow of the Academy of Pharmaceutical Sciences and an Honorary Member of the Royal College of Radiologists.
Professor David Thurston is Emeritus Professor of Drug Discovery in the Institute of Pharmaceutical Science at King’s College London. He has been a member of several national scientific committees including the Projects Committee of Cancer Research UK. He also served on the Cancer Research UK New Agents Committee which oversees the acceptance of novel antitumour agents for development and clinical trial. He is a co-founder of a number of biotech companies including Spirogen, Transcriptogen and Femtogenix. Professor Thurston is a Fellow of the Royal Pharmaceutical Society and the Royal Society of Chemistry.
Dr Chris Martin has been the Chief Executive Officer and Director of ADC Therapeutics since June 2015. Previously, he was Co-Founder of Spirogen Ltd and its Chief Executive Officer leading up to the company’s sale to AstraZeneca in October 2013, at which point he became both a member of MedImmune’s Management Leadership Team and AstraZeneca’s Senior Leaders Group. He is a Fellow of the Institution of Chemical Engineers and a Sainsbury Management Fellow.
This story has been adapted from Coming together for Zynlonta, written by Liam Drew and published by Cancer Research UK on 2 July 2021.